A few weeks back, I did a detailed post about my bicycle called “The machine.” Now it’s time to post about the blob of protoplasm pushing on the pedals. Heads up, it’s a long one.
I wanted to call this post “The modified limited hangout route”, inspired by this hilarious exchange caught on tape in 1973 as Nixon and his deputies try to figure out how much of the Watergate story to tell.
Nixon: “You think, you think we want to, want to go this route now? And the – let it hang out, so to speak?”
Haldeman: “It’s a limited hang out.”
Dean: “It’s a limited hang out.”
Ehrlichman: “It’s a modified limited hang out.”
I’ve never been much for privacy. My life is so boring, I sort of pity anybody who would want to pry into it. Knock yourself out. But I thought it would be interesting to come clean about my body and its medical problems. Let it all hang out, in a modified limited way. As a medical educator, I hope it will be useful to explain these common conditions, and the medications I take for them.
Ruptured disc/S1 radiculopathy. Like most Americans, I suffered from low back pain much of my life. After a particularly vigorous bike ride, the pain took longer than usual to go away, and I suddenly noticed I couldn’t walk on tiptoe. My ankle jerk reflex was also gone, and I was numb on my lateral left foot. I knew what I had before we got the MRI.
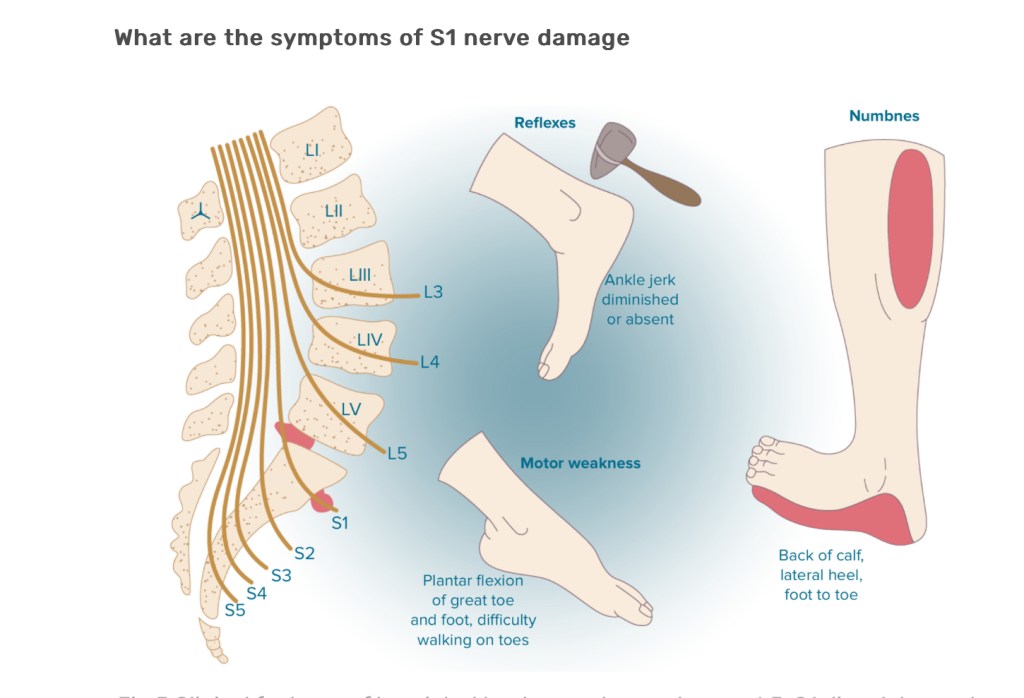
The first sacral nerve, or S1, exits the spinal cord and passes between the fifth lumbar and first sacral vertebrae, going right by the L5/S1 intervertebral disc (discs are the fibrocartilaginous cushions between the vertebrae.) This is the most common disc to rupture, and if it impinges on that nerve, you get some or all of these symptoms. Ruptured discs commonly resolve with conservative care, and I gave it 12 weeks. When I finally had surgery in 2001, the orthopedist commented that my nerve looked pretty beat up. Seven years later, I had similar symptoms on the other side, and this time I wasn’t waiting. I got the MRI on Tuesday, surgery on Wednesday, and was back at work the following Monday.
The pain was never very problematic, what I missed was the motor function of that nerve, which supplies the gastrocnemius muscle in the calf. Now, over 20 years later, I have only 10% of the strength in those muscles I used to have. My lower legs used to look like 10-pins, now they’re more like candlepins. My hiking and biking speed diminished accordingly, I joke that I’m only hitting on two cylinders. This new dropper post is making me pedal in a different way, use my ankles more, and this might constitute belated physical therapy, restoring some of the strength. But I’m not holding my breath.
I should caution people about rushing to MRI for back pain. In one study 100 healthy people with no back pain had MRIs, and 50% of them had ruptured discs. It’s an occupational hazard of being a bipedal primate, we stood up on our hind legs before our spines had evolved. Surgery never makes sense for ruptured discs that don’t correspond to a specific neurological syndrome, in fact it often makes things worse. Conservative care is the treatment of choice in most cases. I was just one of the unlucky ones.
I take no medications for this. When I was in the throes of my second ruptured disc, I staggered maximum doses of ibuprofen and acetaminophen, which controlled the pain and let me do a major hike. It was when I got down that I discovered I had the disc rupture. Pain meds are only a Band-Aid for back pain, they don’t alter the course of the condition, and they can mask important symptoms, never mind the huge risk of side effects and medication dependence. And for me, I feel worse when the medication wears off than I did before I started it. I did the entire Camino with a fair amount of musculoskeletal pain, but never took a single med. Typically, the pain would just ease with ongoing exercise.
Hypertension/cardiovascular risk. Heart disease does not run in my family, I have never smoked, don’t have diabetes. But as an internist, I’m aware that heart attacks and strokes are the #1 and #3 killers of men in this country. On a number of occasions I’ve had odd sensations in my chest that I thought were not cardiac, but confirmed with stress tests and stress echocardiograms, all negative.
Just before I retired in 2020, I noticed my blood pressure was running a bit high, I got a home cuff and found I was averaging about 142/85. Though I could be better with my diet, my exercise is quite good and I felt I was doing a reasonable job with nonpharmacologic management. Well over half of American men over 60 have hypertension, and should be on medication. Ongoing research has demonstrated the goal should be under 130/80.
There are many medications to control hypertension. Diuretics cause the kidneys to lose salt and fluid. Beta blockers slow the heart rate and contractility. Calcium channel blockers relax the smooth muscle in the walls of your small arteries (arterioles), and relieve pressure by vasodilation. It’s like trying to reduce the water pressure in your house, you can either bleed off fluid, turn down the pump, or open up all the spigots.
All of these medications have side effects. A relatively new approach is to target your body’s hormone angiotensin, which raises blood pressure by constricting blood vessels and causing the kidneys to retain salt. Angiotensin can be reduced by inhibiting the converting enzyme (enzymes are proteins your body makes that catalyze or facilitate chemical reactions) that activates it with angiotensin converting enzyme inhibitors, or ACE inhibitors. Unfortunately, these cause a cough in over 10% of patients. Easier to tolerate are angiotensin receptor blockers (ARBs), which block the effect of angiotensin on the blood vessels and kidneys. I take the ARB olmesartan (Benicar) and have tolerated it well, with good effect on the BP.
The other cardiac risk factor to control is cholesterol. My numbers have always been quite good, but not perfect. An evidence-validated tool is the ASCVD risk calculator. https://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/ My risk of a heart attack or stroke in the next 10 years was in the 10-15% range, high enough to merit statin therapy.
Statins reduce cholesterol by inhibiting the enzyme that synthesizes it, HMG-CoA reductase. It is the rare man over 60 who would not benefit from them. Well over 30 years of research have borne this out. Statins are so commonly prescribed that their side effects get a lot of press, and many are leery to take them. But the vast majority can tolerate them without difficulty, and substantially reduce their cardiac risk. I take atorvastatin (generic Lipitor) 20 mg daily. My cholesterol plummeted, as it always does, but more importantly my risk improved. Zero side effects, I just have to avoid grapefruit, which interacts with the enzyme.
Celiac disease. I’ve been giving blood for years, but lately was rejected because my hemoglobin was too low. Not uncommon, figured I would just stop donating, and take an iron supplement.
But it didn’t get better, and my ferritin level, a more accurate measure of iron stores, was half normal. That’s alarming in a male, suggests that I am losing blood somewhere, most commonly from the G.I. tract. Ugh. That meant I needed a colonoscopy and an upper endoscopy, looking for a bleeding ulcer or tumor.
My sister has celiac disease, and it runs in families. With great reluctance, I asked for the screening test, Tissue Transglutimase Antibody (TTAb), even though I had no symptoms. It came back 10 times normal. I was reasonably awake during the upper endoscopy, and saw the duodenum (upper small intestine) looked grossly normal, but biopsies were taken.
I was waiting in line at Starbucks when the email came with the results. I ate the croissant anyway, possibly my last one, and insisted on reviewing the slides with the pathologist face-to-face.
Your small intestine, you may remember, is where most of your food gets absorbed. To increase the surface area, it is lined with finger-like projections called villi. People with celiac disease have an allergy to gluten, a protein in wheat, rye, and barley that causes small intestinal inflammation which gums up or obliterates the villi.

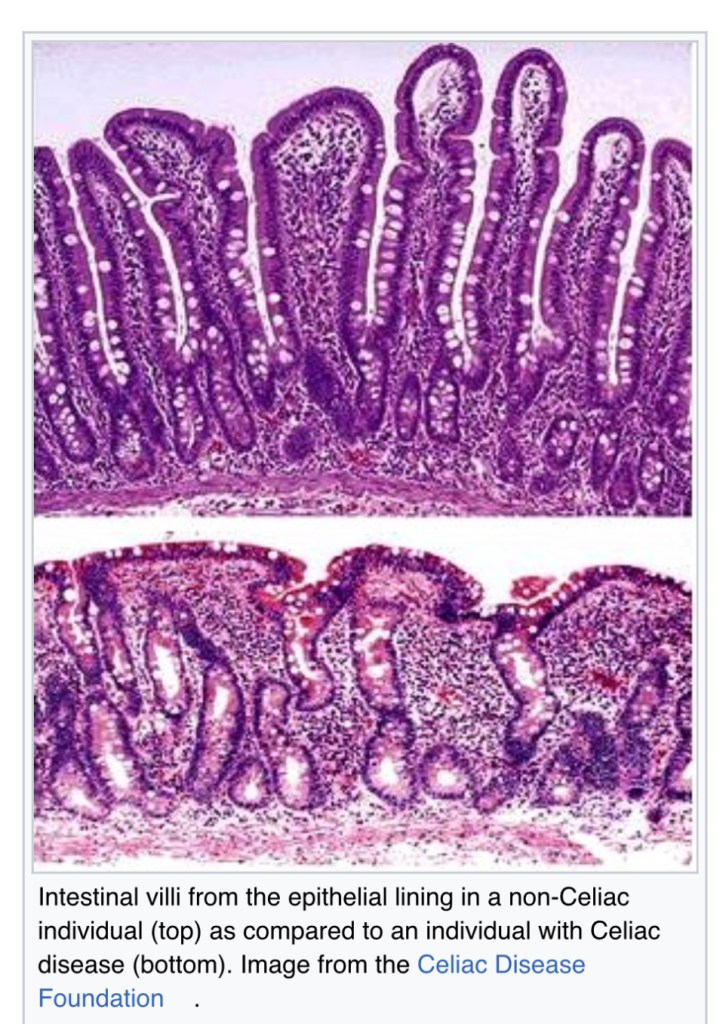
In medical school we were taught that celiac disease (AKA sprue) was rare, causing severe malnutrition and making one poop vast quantities of fat, called steatorrhea. Since then we’ve found that the estimated global prevalence of celiac disease based on serologic studies is ~ 1 percent, and that most people have milder symptoms. In my case, the only symptom was not being able to absorb iron. Reluctantly, I started avoiding gluten, didn’t really feel any different, although a long-standing symptom, night sweats, went away. A hematologist later confirmed he has seen this commonly. The condition is improving, but not completely. I must confess I am not 100% adherent to the diet, it’s especially challenging when on the road and eating primarily out of convenience stores. I continue to take iron daily, and have had infusions of intravenous iron.
Gastro-esophageal reflux disease (GERD). I’ve had heartburn most of my adult life, along with 50% of the population. It didn’t get much better on the gluten-free diet. Endoscopy did not show anything worrisome, but I found I need to take a proton pump inhibitor (PPI) to control my symptoms.
I’m “sure” you remember from chemistry class that acids are basically free protons (hydrogen ions), hydrochloric acid in this case, secreted by cells that pump those protons into your stomach.

Those pumps are powerful, the pH (the negative logarithm of hydrogen ion concentration) of stomach acid ranges between 1 and 2, low enough to eat through bone—your gastric lining protects your body from its corrosive effects. PPIs mitigate this acid production, I take omeprazole (Prilosec), at one time the most prescribed medication in the world, along with calcium carbonate (TUMS) at bedtime.
PPIs are generally quite safe, though there’s some concern about an association with dementia. I do the NYT crossword daily to make sure I’m not losing it. Speaking of losing it, weight loss would help my GERD.
Hair loss. At age 47, friends were telling me I was getting a little thin on top. By then minoxidil (Rogaine) was generic and cheap. Once prescribed as a last-resort hypertension medication, minoxidil caused lots of side effects, one of which was hair growth. Applied topically, it acts as a vasodilator, improving blood flow to withering hair follicles. It works best for vertex baldness, avoiding the Friar Tuck look.
More recently I noticed my hairline was receding in a widow’s peak or male pattern baldness pattern, with testosterone having a significant role. In the 1990s, an anti-testosterone drug, finasteride (Proscar, a 5α-reductase, interferes with the last step of the hormone’s synthesis) was introduced to mitigate prostate swelling and symptoms. Like minoxidil, hair growth was noted as a side effect, and took place even at a fifth the dose (1 mg) with less sexual side effects. Finasteride was rebranded as Propecia, the patent renewed, and the price jacked up. Currently it’s $319 for a 90 day supply, not covered by insurance, since it’s a cosmetic drug. But the original Proscar has been generic for years, retail cost $4 for a 90 day supply. I just take one tablet every five days.
I’m not sure my hair has gotten any thicker, but it doesn’t look bad for someone who first noticed hair thinning 26 years ago. The Friar and the widow seem to be held at bay.
So for a healthy guy who doesn’t like taking drugs, I’m on quite a list of medications: olmesartan 40 mg, atorvastatin 20 mg, omeprazole 20 mg, iron 65 mg, calcium carbonate 400 mg, all daily; finasteride 5 mg every five days, and topical minoxidil daily. Total cost about $10 per month, no side effects, still able to do things like this bike trip.
I guess the point of this “modified limited hang out” is to show that older folks needn’t fear medications, in many cases the cost and side effects are minimal, and hardly limiting at all. Meantime, quality and length of life can be significantly improved.
©️ 2024 Scott Luria
Love your honesty and also patient friendly breakdown of common medical problems that ail you (and many Americans)! Educating and empowering patients with knowledge even in retirement Scott! This is great!
LikeLike